Patient Impact Stories
True stories of harm and benefit when patients can and can't see what's in their chart

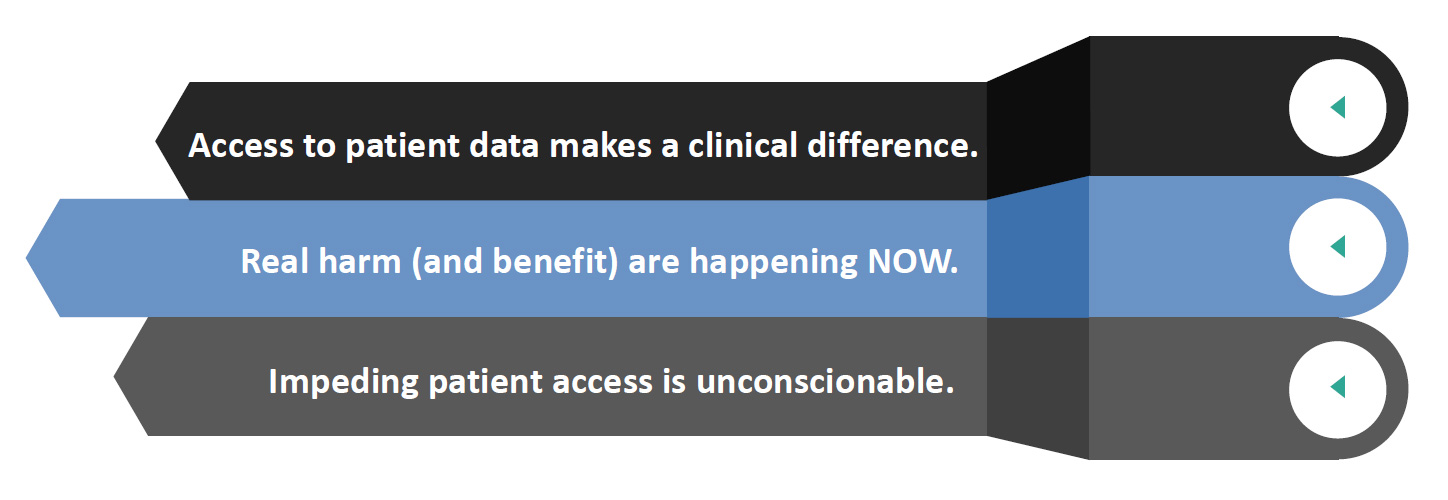
Harm can result when patients and carepartners cannot see, collect, collate, and verify information about their cases.

But good can result when patients and carepartners CAN see, collect, collate, and verify information about their cases.


Welcome to Unblock Health's Patient Impact Stories: true stories of harm & benefit.
Suffering
Regina's husband Fred was denied pain medicine for his metastases, and food, for hours at his new hospital because his records had not been sent along. Here she is painting a mural of his final days, after his death.

Death
Sue Sheridan's husband Pat died at 45. Office staff had misplaced a pathology report identifying his malignant spinal tumor so the doctor never saw it.
Stress and Labor
Morgan Gleason's records are scattered across 23 portals; no provider anywhere has the full picture. "I had to spend hours requesting records from 12 doctors - while unwell."


Delay and Suffering
Amy had kidney stone treatment delayed "three painful days and four sleepless nights" while her doctors tried to retrieve her records.

Stress and Labor
Sue, mom of rare disease patient Kristen, was unable to get critical appointments for her child until she laboriously assembled the previous records herself.

Labor and Uncertainty
Adrian manages care for his elderly mother 200 miles away, who sees doctors in six practices that use EMRs from different vendors. Coordination for best possible care and to avoid costly mistakes is impossible without full data access.

Delay and Risk
Janice's mammogram showed an issue, but she was never notified to come in for a follow-up visit.
Her next mammogram was delayed - because she hadn't done the follow-up that she didn't know about!

Risk and Suffering
Former police officer Bray has multiple allergies and implanted devices, and is treated at five health systems. No one has her comprehensive record. Continued...

Risk and Suffering
Bray was seriously injured in a recent high speed stoplight accident. She declined ambulance transport & treatment out of concerns of being harmed at an unfamiliar hospital that didn't have her records.

Lost Records, Uncertainty
Stacey was diagnosed with breast cancer after her first mammogram. She tried to get her previous records from another state, including previous breast issues. She had a difficult time getting them, and then was told they'd been destroyed.
Labor, Delay, Uncertainty
7 year old Bailey nearly died from a drug contraindication. Today her information is scattered across seventeen portals.
Bailey's mother, Kristen, has had to repeat her daughter's medical history to every new doctor, a horrible patient experience and error-prone workflow.


Delay, Suffering, Death
Stacy is a patient advocate with 20 years of experience as a healthcare executive. She still has trouble obtaining records that her clients are legally entitled to.
Three patients she was assisting have died during delays awaiting records to seek second opinions.
Catastrophic Errors Impacting Patient Safety
Heart patient "G" went to a new doctor. Lacking a complete history, she had to repeat her story again. She included that her previous surgeon was questionable - he'd been arrested by the FBI in the O.R., accused of running a drug ring.
Reviewing the transcript, she found they'd written that she had arrested in the OR - a major error affecting possible choices of future treatments.
Generic photo from CBS - not the actual event

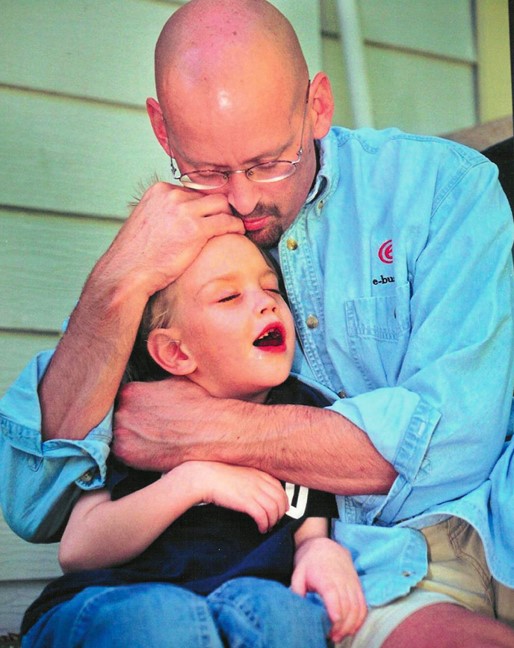
Stress & Labor
While being treated for his own leukemia diagnosis, Vincent's 10 year old son was diagnosed with Ewing sarcoma which required an extensive care team, 2 years of aggressive treatment, and the amputation of his right leg at the knee. Managing the health information of 2 patients with cancer was next to impossible. Contributing data to advance research for his son's rare disease was hopeless. He created an app, Andaman7.

Stress & Physical Harm
Alicia needed to get a vacuum-assisted biopsy which required her to deliver her images, actual films, from Tufts to Boston Medical Center (BMC). She slipped and fell on the ice in front of BMC. The films landed in a snowbank and got wet. She was worried she would need to have the imaging redone and then, even worse, pay for them out of pocket. Why are patients hand-delivering images to their hospitals to get the care they need?

Medical Error & Delayed Diagnosis:
Erika's barium enema X-ray was initially incorrectly reported as unremarkable, delaying her late-stage colorectal cancer diagnosis by 6 months.
Six months later, Erika's surgeon showed her her X-ray and report. Had she seen these initially, she would've known that her tumor was literally choking her colon. She and her surgeon were outraged.
Erika says it should be standard practice for doctors to review both the actual imaging and the corresponding report WITH patients and to give them access to both.


Delay and Wasted Expenses
Betty is a 74 year old lung cancer patient who went to MD Anderson for expert treatment. Her doctor rushed the requested printouts of her chart by FedEx.
The shipment got lost, which was going to require cancelling the appointment.

Delay and Suffering
If Kistein had access to her medical records when she needed them, she could have coordinated her care seamlessly and safely.
By not having access to her medical records, Kistein suffered in medical crisis, living with crippling pain for over three years as well as enduring painful injection therapy.
Delays in Care, Suffering, Death
Debi’s 93-year-old mother, Ruth, lived 6 hours away in a memory care facility. After a fall, Ruth was assessed by her caregivers. Due to COVID-19, it was determined her injuries were not serious enough for the ER.
Still in pain 2 days later, Ruth was brought to the ER. The ER doctor reviewed her imaging and said nothing was broken. Ruth was sent back to the memory care facility.
Debi knew something was not right. Her mother was still in pain and not walking properly. Ruth’s patient portal only had the ER Discharge Document and did not have any of the imaging reports from Ruth’s ER visit. Debi needed to see the imaging reports.

Delays in Care, Suffering, Death
Debi used a FHIR based app, MyLinks, to review the imaging report herself. The report stated Ruth’s hip was broken. The information given to Debi over the phone and the ER Discharge Document on the portal were wrong!
Debi desperately advocated for an emergency surgery which was finally scheduled 8 days after Ruth’s fall. The surgery revealed severe damage to the surrounding muscles and tissue from delays in receiving care.
Ruth did not recover from the emergency surgery and died.

However...
Good can result when patients and carepartners CAN see, collect, collate, and verify information about their cases.

Patient Access using FHIR Can Save Lives
Patients now have the right to gather their data from hospitals and clinics using any FHIR application of their choice. In most cases, these FHIR applications have more information than what is available in a portal.
It is so critical for patients and caregivers to have access and copies of all their records. This information can help save lives.

Patient Access: Prevents Delays and Expenses
Betty had wisely brought copies (laboriously assembled) of her data and images, so the visit went on, avoiding weeks of delay and redundant travel costs.


Patient Access: Prevents Medical Errors
89 year old Anne discovered that a new eye doctor's office had wrongly charted her as diabetic, which led the doctor to wrongly order surgery.
It would have caused immense family stress, time in caregiving, risk, and needless expense. But she caught it.

Patient Access: Prevents Medical Errors
When Anne entered rehab after a hip replacement, her caregiver daughters spotted a transcription error (hyper ↔ hypothyroid) and got it fixed, preventing a disastrous mistake by some physician who would have been obeying bad chart data. Patient access saved the day.
Patient Access: Prevents Errors & Omissions
Grace has an anaphylactic morphine allergy. She rigorously checks to see that the allergy is listed in every new provider's chart. It often isn't. She fears an unexpected ER visit.
She wants a single record that's available everywhere.

Patient Access: Prevents Complications, Suffering, Costs
When Morgan went to college and moved hospitals, she brought the protocol she'd developed for years with her doctor after she got meningitis (painful and harmful) as a side effect of her treatment.
By showing her new doctor the written plan, she was able to advocate for herself and get the right treatments, avoiding recurrence (and costs) of meningitis.
Patient Access: Provides Choice & Autonomy
Casey learned of her breast cancer recurrence from an MRI report in her patient portal. As a patient, she wants to know everything about her health ASAP.
Some people may want results delivered via clinician verbally but for Casey, getting results as soon as they are available is her choice. Casey says, "Preferences of the patient are the primary priority."